Ming-Qing Du, MB, PhD, FRCPath
Department of Pathology
University of Cambridge
THYROID MALT LYMPHOMA: SELF-HARM TO GAIN POTENTIAL T-CELL HELP
Date: 28 October 2021
Time: 8:00 – 9:00 PST | 11:00 – 12:00 EST | 16:00 – 17:00 GMT
Location: Webinar
Summary
Learning Objectives
- Learn about a multidisciplinary approach to investigate thyroid MALT lymphoma that utilized targeted gene sequencing and digital pathology image analysis
- Learn how HALO can be used to perform proximity analysis on multiplexed immunofluorescence images to investigate spatial relationships between CD20, CD4, PD1, and CD69
- Learn about downstream consequences of inactivation of CD274 (PD-L1) and TNFRSF14 in thyroid MALT lymphoma
This webinar is ideal for researchers in oncology, immuno-oncology, pathologists, attending physicians, image analysts, and others working in digital pathology.
Presenters
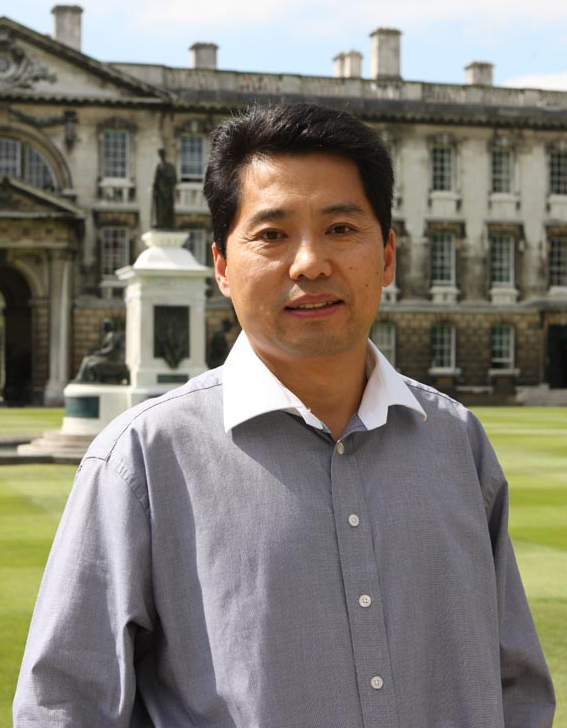
Dr. Du is a Professor of Oncological Pathology and Consultant Molecular Pathologist, Addenbrooke’s Hospital, University of Cambridge since 2003. He is also a Fellow of Hughes Hall, University of Cambridge.
He obtained his MB from Hebei Medical College, P.R. China in 1984, and subsequently PhD from King’s College Hospital School of Medicine and Dentistry University of London in 1990. After a three-year postdoctoral fellowship at the Institute of Cancer Research, Sutton, UK, he joined Professor Peter G. Isaacson’s research laboratory at Department of Histopathology, University College London in 1993. In August 2003, he joined the Department of Pathology, University of Cambridge and has been working there since then.
He and his colleagues have made a series of seminal contributions to our current understanding of the molecular pathology of MALT lymphoma, splenic marginal zone lymphoma, diffuse large B-cell lymphoma and angioimmunoblastic T-cell lymphoma. He is a highly cited clinician scientist with over 220 research publications, a Hirsch index of 76 and a total of 20260 citations (September 2021). In 2013, he was awarded the Goudie Lecture and medal by the Pathological Society of Great Britain and Ireland to recognise his research achievements.
