Tumor-specific tumor-resident cytotoxic T cells predict recurrence in stage III melanoma patients treated with adjuvant immunotherapy
Date: 10 December 2021
Time: 8:00 – 9:00 PST | 11:00 – 12:00 EST | 16:00 – 17:00 GMT
Location: Webinar
Summary
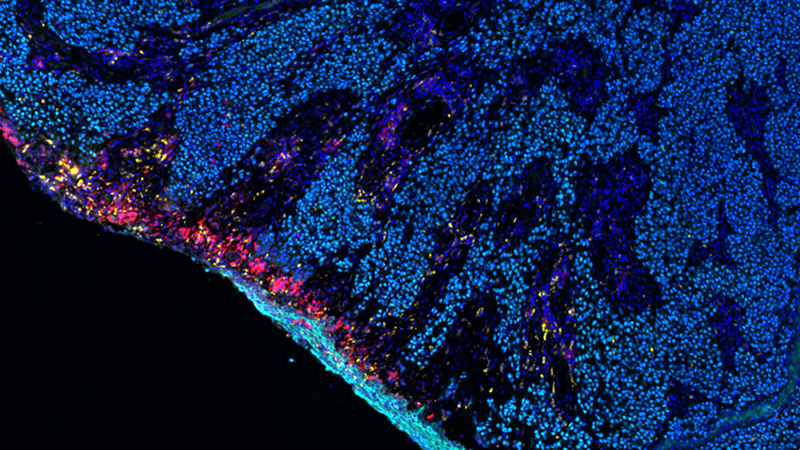
Two CD8+ T cell subpopulations were significantly associated with recurrence disease recurrence on adjuvant immunotherapies. First, tumor-specific, resident T-cells (Tsrm) comprised a significantly higher proportion of CD8+ T cells in recurrence-free patients (P = 0.0004). Conversely, bystander T-cells comprised a significantly greater proportion of T-cells in patients who developed recurrence (P = 0.0002). Spatial analysis identified that Tsrm localized significantly closer to melanoma cells than bystander T-cells. Multivariable analysis confirmed that low Tsrm proportions and other clinical factors were associated with recurrence. The final Cox regression model identified patients who developed recurrence with an AUC of 75.9% in the discovery cohort and AUC of 69.5% in a separate validation cohort.
Pre-treatment Tsrm cells are strongly associated with a reduced risk of melanoma recurrence in adjuvant-PD-1-treated patients. This population may not only represent a biomarker for recurrence following anti-PD-1 therapy but also be an avenue for therapeutic manipulation and enhancing outcomes for cancer patients treated with immunotherapy.
Learning Objectives
- Learn how cellular phenotyping combined with spatial analysis provides insights into stratifying melanoma patient populations
- Learn which cytotoxic T-cell populations are predictive of recurrence in anti-PD-1 treated high risk state III melanoma patients
- Learn how HALO and HALO AI collaborate to perform tissue and cell segmentation, quantification of T-cell subsets in tumor regions, and spatial analysis
This webinar is ideal for cancer researchers, pathologists, attending physicians, image analysts, and others working in digital pathology.
Presenters

James Wilmott, PhD
NHMRC investigator fellow | Senior scientist
The Melanoma Institute Australia, The University of Sydney
Senior lecturer James Wilmott is the research leader of the Translational Melanoma Research Group of the Melanoma Institute Australia, The University of Sydney. Dr Wilmott is a current holder of an NHMRC early career fellowship and received his PhD in 2013 from the University of Sydney. Dr Wilmott is recognized internationally as an emerging expert in clinical implications of genomic profiles (First author Nature and Int J Cancer), immune profiling of cancer tissue (Co-author in Nature, The Lancet Oncology, senior author in Clinical Cancer Research and Oncoimmunology) and in biomarkers of response of systemic therapies (Senior author Cancer Cell). Dr Wilmott has amassed over 169 publications since 2016 in the top medical journals, including: twice in Nature, twice in Nature Cancer, once in Cell, twice in Lancet Oncology, once in Cancer Cell and eleven times in Clinical Cancer Research and six times in Nature communications. With over 18,230 citations, with 43 articles with >100 citations and a H-index of 56. As a translational research scientist, Dr Wilmott has worked closely with clinical groups to identify areas of need, find a solution and work to implement findings into improved patient outcomes.